New technology was used during deep brain stimulation surgery, allowing for sensing of local field potentials in conjunction with segmented intracranial leads.
The patient
A 63-year-old woman was diagnosed with Parkinson’s disease eight years earlier, after developing stiffness of the right arm and leg while undergoing treatment for breast cancer. She then developed tremor of the right thumb, and ultimately was diagnosed with Parkinson’s disease. After physical therapy did not provide adequate relief, the patient started medical therapy for her motor symptoms of slowness, stiffness and tremor. Over the years, six other Parkinson’s medications were either trialed or considered, and the patient’s medication regimen was complex: She was taking levodopa every two hours and still had continued periods of early wearing off of medications, leading to rapid fluctuations in her motor control. These fluctuations affected her ability to enjoy volunteering and gardening, and required careful timing of her meals around frequent medication doses. Painful dystonic cramping of the feet also became refractory to oral medications and Botox injections.
The challenge
Medications were now no longer providing the patient with adequate and consistent resolution of the bradykinesia, rigidity and tremor she experienced from moderate-stage Parkinson’s disease. Her medications wore off before the next dose was due, despite taking frequent doses. Frequent and high-dose medications also were causing dyskinesias, or excessive movements.
The physicians

Abigail J. Rao, M.D.
Neurosurgeon
Norton Neuroscience Institute
Justin T. Phillips, M.D.
Neurologist
Norton Neuroscience Institute
The solution
After extensive consideration of deep brain stimulation (DBS) therapy, the patient was evaluated by Norton Neuroscience Institute’s multidisciplinary movement disorders team. In addition to consulting with her neurologist and neurosurgeon, the patient was evaluated by Parkinson’s-trained speech therapy, occupational therapy, physical therapy and neuropsychology specialists. These evaluations inform the risk-benefit analysis of proceeding with DBS. Ultimately, we recommended DBS.
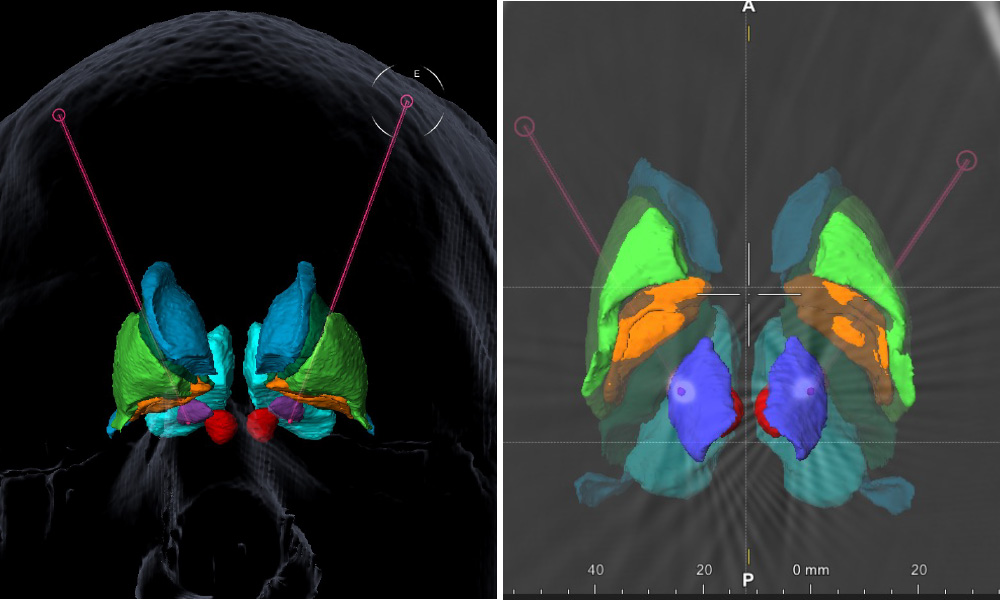
DBS, targeting the subthalamic nucleus (STN), was performed, to modulate the central motor circuitry affected in Parkinson’s disease. The surgery was performed using high-resolution MRI to directly visualize the target, and stereotactic surgery techniques to place a 1.27 millimeter diameter lead within the intended target, which is about 1 cubic centimeter in volume (Figure 1).
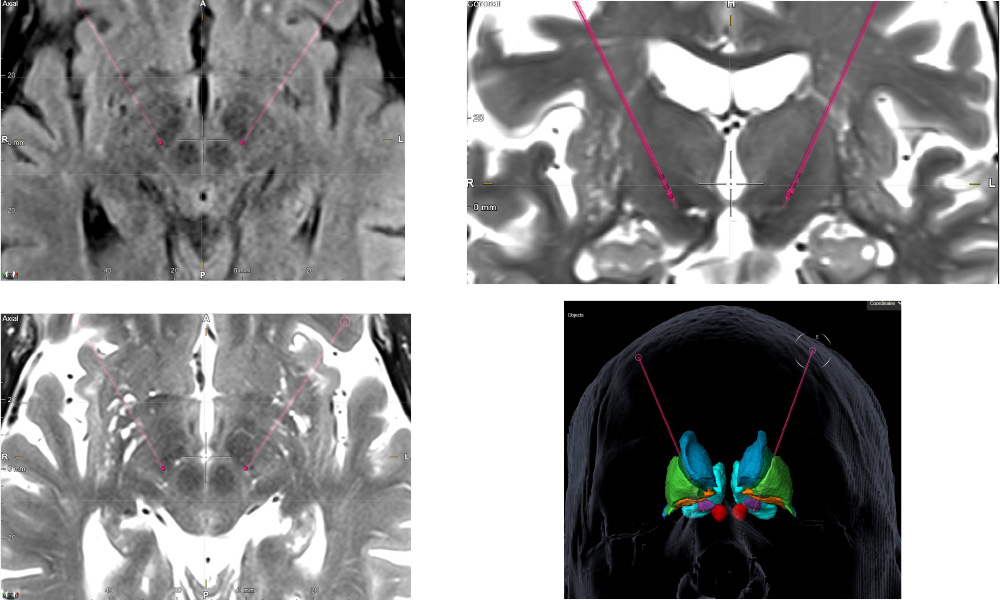
The surgery was performed under general anesthesia, which has been correlated with an improved safety profile, including lower rates of hemorrhage and postoperative speech delay. Historically, techniques relied on the patient being awake during surgery. Intraoperative CT scanning was used for confirmation of lead placement and evaluation of intraoperative hemorrhage or brain shift.
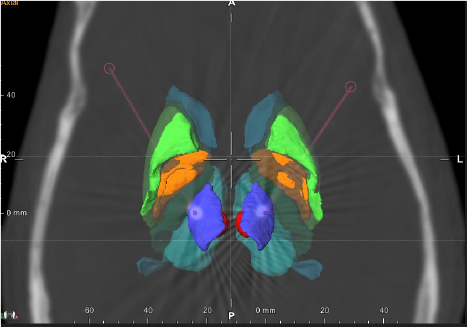
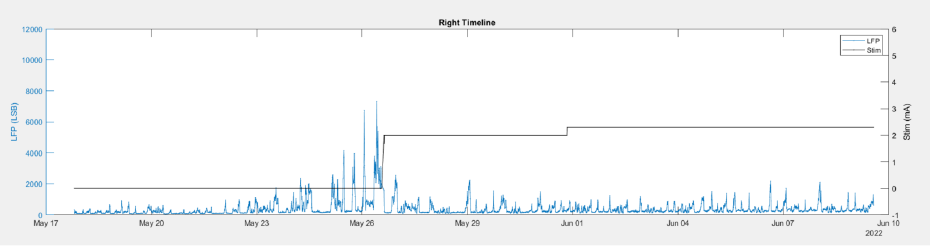
New technology was used allowing for sensing of local field potentials, known to correlate with abnormal movements in Parkinson’s disease, in conjunction with segmented intracranial leads that allow for directing the electrical stimulation field toward the target of interest and away from the neighboring off-target nuclei.
The result
Total surgical time was 2.5 hours. The patient was discharged the next day. She experienced minimal surgical pain and no other surgical complication. She met with her neurologist about two weeks after surgery for initial programming. After optimization of the programming and medications over the next few months, medications were reduced by more than half, and she experienced fewer motor fluctuations, less dyskinesias and dystonias, and better enjoyment of her daily hobbies. These improvements in motor symptoms correlated with a change in the pattern of certain local fields potentials. This concept is the basis for newer technology that detects and stores local field potential data, which can be reviewed by the patient’s neurologist and used to help guide programming the DBS.
Treatment and results may not be representative of all similar cases.
Refer a patient
To refer a patient to Norton Neuroscience Institute, visit Norton EpicLink and open an order for Neurosurgery or Adult Neurology.

