Dementia needs to have cognitive impairment that leads to a functional impairment or a loss of independence in instrumental activities of daily living.
Diagnosing dementia in primary care and other practices starts with evidence of cognitive decline from a previous level of performance in one or more cognitive domains, according to Rachel N. Hart, D.O., a geriatric medicine specialist at Norton Neuroscience Institute.
“Dementia really needs to have cognitive impairment that leads to a functional impairment or we need to have loss of independence in instrumental activities of daily living and/or our activities of daily living,” Dr. Hart said in a recent continuing medical education opportunity.
The diagnosis needs to start with concern from the patient or someone close to them such as a family member, caregiver or health care provider.
Related: Dementia care for communities of color
The criteria would be substantial impairment in cognitive performance in at least one of the following:
- Complex attention
- Executive function
- Learning and memory
- Language
- Perceptual motor skills
- Social cognition, or processing information about other people and social situations
Cognitive assessments for diagnosing dementia in primary care
- Montreal Cognitive Assessment. This is one of the most highly regarded tests, but may not be practical in the primary care setting because of the amount of time required.
- Mini-Mental State Examination. This is the most widely used test for assessing dementia, and takes 10 minutes or less to complete.
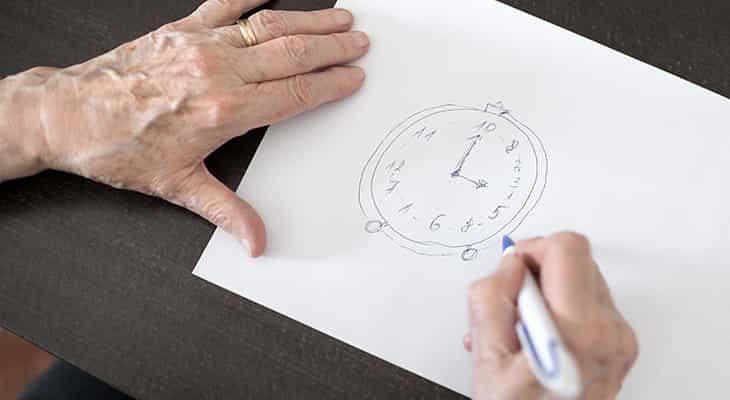
- Mini-Cog. This is a three-item recall test with a clock draw test that requires the patient to place the numbers on a preprinted circle, then draw the hands to indicate a given time.
For dementia to be diagnosed, the condition needs to interfere with everyday activities, not just present itself in the context of delirium, and escape description by another mental disorder such as depression.
Refer a patient
Use Norton EpicLink to quickly and easily refer a patient to Norton Neuroscience Institute.
Symptoms can include:
- Aphasia – Difficulty finding the right words
- Apraxia – New difficulty using common tools like the telephone or television remote control
- Agnosia – An inability to recognize formerly familiar items or familiar people
“A decrease in executive function can manifest itself in a task such as balancing a checkbook,” Dr. Hart said.
Reversible causes of cognitive impairment need to be considered as well. There are standard tests such as blood counts, metabolic panels, vitamin B12 level, folate level and brain imaging — preferably a magnetic resonance imaging (MRI) scan — that should be checked. Other tests that may need to be considered are based on a patient’s risk factors and can include syphilis serologies, a Lyme disease titer, an HIV test, heavy metal assays, an EEG or a lumbar puncture.

