Cerebral palsy affects thousands of children every year. Here’s what you should know about classification, diagnosis and more.
Cerebral palsy is one of the most common disabilities affecting children. It is a group of permanent conditions and symptoms that affect movement, posture, overall mobility, gross motor skills, manual ability, vision, speech and muscle tone. Movement disorders such as this are often accompanied by disturbances in sensation, cognition, communication or behavior. Some statistics about cerebral palsy include:
- The prevalence of cerebral palsy in the U.S. is 1 out of 345 children.
- Cerebral palsy diagnosis typically doesn’t occur until a child is 2 to 3 years old.
- Cerebral palsy is more common in boys than girls.
- Cerebral palsy is more common in African American children than in white children.
- Children with low birth weight are more likely to develop cerebral palsy.
Cerebral palsy can be caused by genetic mutations, an event during pregnancy, birth injury during labor and delivery, or asphyxia. After birth, brain damage, trauma, injury and illness such as meningitis can cause cerebral palsy.
A recent continuing medical education session for a pediatric primary care audience addressed what providers should know about diagnosing or treating children who have cerebral palsy.
Catherine P. Schuster, M.D., pediatric physical medicine and rehabilitation specialist at Norton Children’s Physical Medicine & Rehabilitation, affiliated with the UofL School of Medicine, discussed classification of the condition and rehabilitation treatment strategies. Her presentation explored recommendations for treatment plans based on severity, underlying pathology and anticipated function. She discussed other system involvement and how that affects treatment, as well as the need for a flexible treatment approach as symptoms progress and the patient ages.
Physical medicine and rehabilitation (PMR) and CP
The goal of PMR is to restore physical ability and quality of life for patients with conditions such as cerebral palsy. Dr. Schuster’s approach to PMR looks at the child within the broader context of their cerebral palsy symptoms, environment, support and other factors to create a “big picture” view of the patient.
Importance of accurate cerebral palsy diagnosis
According to Dr. Schuster, an early and accurate cerebral palsy diagnosis can benefits for the child and family including:
- Giving the family and the entire medical team an idea of what to expect as the child develops and the condition progresses
- Allowing early intervention for better outcomes
- Preventing unnecessary investigation
- Accessing earlier support and resources
- Potential implications for future family planning
Cerebral palsy mimickers
There are some conditions that initially can present similarly to cerebral palsy.
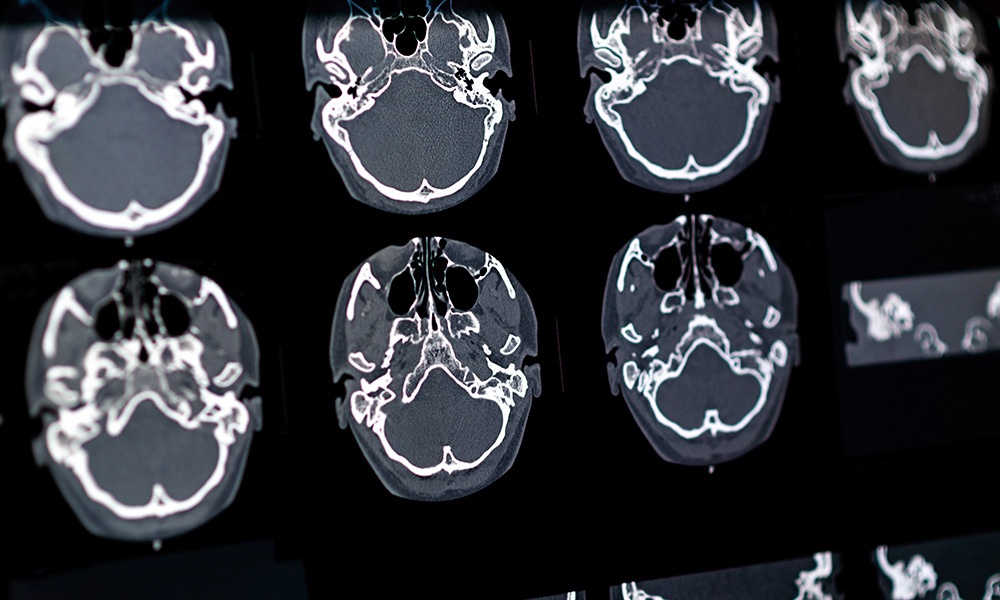
“A mimicker is when you have a condition that may have some cerebral palsy symptoms, such as spasticity, ataxia or dyskinesia, but you don’t have the risk factors or the neuro imaging findings consistent with a history of a brain injury or congenital malformation,” Dr. Schuster said. “It is estimated that imaging is reported to be normal in up to 15% of children who have an established cerebral palsy diagnosis.”
According to Dr. Schuster, these tools have the most accurate diagnosis, especially when used in conjunction and with clinical reasoning and judgment:
- MRI
- Prechtl qualitative assessment of general movement
- Hammersmith Infant Neurologic Examination
Refer a patient
To refer a patient to Norton Children’s Neuroscience Institute, visit Norton EpicLink and open an order for Pediatric Neurology.
Classification of cerebral palsy
“Once accurate diagnosis is determined, and mimickers are ruled out, we determine the classification of cerebral palsy, and screen for associated conditions,” Dr. Schuster said.
The three aspects of classification are:
- Type of movement disorder: spastic; dyskinetic or dystonic; or ataxic
- Anatomic distribution: how many limbs affected by symptoms
- Function: how the movement disorder affects the child and their quality of life
Those with spastic cerebral palsy may focus on stretching the muscles, tendons and ligaments of the limbs. Dyskinetic or dystonic refers to abnormal involuntary movement. This can include abrupt twisting or repeated movement that can be painful. Ataxic cerebral palsy refers to difficulty with balance, proprioception or coordination.
“By understanding the underlying classification, it allows families to know what to expect in terms of that child’s prognosis and quality of life,” Dr. Schuster said.
Prognosis based on cerebral palsy classification
“One of the first things families want to know about a child with any type of motor function impairment or movement disorder, after a cerebral palsy diagnosis, is when will they walk,” Dr. Schuster said. “For prognosis for ambulation, we look at the presence or absence of primitive reflexes, how their gross motor skills are developing, and then the type of cerebral palsy.”
This kind of conversation should be covered over several visits, and providers should be clear about what sort of physical assistance a child might need to walk, and — in general — what the family can expect.
Disorders associated with CP
Any body system can be affected by cerebral palsy, and the likelihood of other system impact increases with the severity of brain damage.
“It is estimated that visual impairments can occur in visual impairments in up to 100% of children,” Dr. Schuster said.
That includes any visual issue, from having amblyopia to having complete cortical visual impairment.
“Hearing impairments and cognitive issues, including lower IQ and executive functioning impairments, are common,” Dr. Schuster said. “Seizures and epilepsy, nutritional deficiencies and low bone mineral density are also things to keep in mind.”
Goals of treatment
The ultimate aim of PMR is to restore mobility and functional ability, and improve quality of life. A child may be referred to specialized interventions and treatments including:
- Physical therapy
- Occupational therapy
- Speech therapy
- Assistive devices, such as a brace, manual wheelchair or other adaptive equipment
- Recreation therapy
- Surgery
- Medication
For any of the cerebral palsy signs or symptoms, such as the most common — spasticity — the family’s goals, resources and lifestyle are important to consider.
Medication interventions for CP
The efficacy of medication on all classes of cerebral palsy depends on the type of cerebral palsy and the individual.
Spasticity: Benzodiazepines are commonly used medications for this movement disorder, especially in young children who already have severely developing spasticity. These medicines have benefits and challenges as well, such as dosing and method of delivery.
- Baclofen is a common antispasticity medication that is typically in pill format, but is available but difficult to obtain in suspension.
- Dantrolene is a peripherally acting antispasticity medication that doesn’t have the sedative side effects of benzodiazepines or baclofen, but liver function must be monitored. And as a liquid formulation, it can be very difficult to dose.
- Tizanidine and clonidine are alpha agonists and have an impact on spasticity control.
Chemodenervation uses injections to help with spasticity management. Some of these are botulinum toxins approved by the U.S. Food and Drug Administration for this use.
Alcohol blocks use 3% to 5% alcohol to denature the motor point of specific nerves to weaken the contraction of the muscle.
Aging and cerebral palsy
Cerebral palsy doesnt get better or go away as a patient ages, and eventually the pediatric patient becomes an adult patient.
“The same issues people without CP have are also present in those with the disorder,” Dr. Schuster said. “Patients who are aging into the adult system will need traditional health screenings such as colonoscopies, but also more specific services such as pain management, adaptive equipment recommendations, physical assistance and more.”
There are roughly 400,000 adults living with cerebral palsy in the U.S. with spastic cerebral palsy, ataxic cerebral palsy, dyskinetic cerebral palsy, and across the entire spectrum of diagnoses. The overall survival rate at 30 years is about 87%. Having intellectual disability or epilepsy can have a negative impact on survival. It is estimated that mobility declines in at least 25% of adults with cerebral palsy.
In summary, cerebral palsy is a brain injury that occurs in utero or within the first few years of life. Classification is based on function, movement disorder and affected limbs. Treatment must include input from the family and a multidisciplinary health care team.